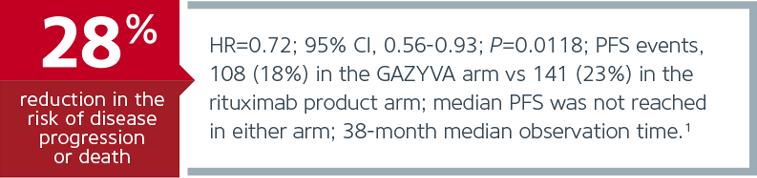
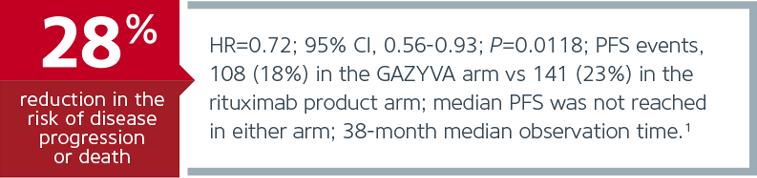
| GAZYVA Is the First and Only Approved Therapy That Demonstrated Superior PFS vs rituximab product in Previously Untreated FL1 |
| With chemotherapy* for stage II bulky, III, and IV patients |
| Primary Endpoint: PFS (IRC-assessed)1 |
 |
|
| Early progression of FL predicts poor prognosis, but early progressors may be difficult to identify in advance2 |
 |
 |
 |
|
 |
| GALLIUM: The Largest Trial in Previously Untreated Follicular Lymphoma (FL)1 |
| • | 1,202 untreated FL patients studied (Grades 1-3a, stage III/IV or stage II bulky disease [≥7 cm]) |
| • | Patients randomized to receive GAZYVAa or rituximab productb in combination with chemotherapy for 6 or 8 cycles, followed by either GAZYVA or rituximab product monotherapy every 2 months for up to 2 yearsc |
| • | GAZYVA and rituximab product were combined with bendamustine (57% of patients), CHOP (33%), or CVP (10%)‡ |
|
|
|
|
| IMPORTANT SAFETY INFORMATION (CONT'D) |
| Warnings and Precautions (cont'd) |
| Progressive Multifocal Leukoencephalopathy (PML) |
| • | JC virus infection resulting in PML, which can be fatal, was observed in patients treated with GAZYVA. Consider the diagnosis of PML in any patient presenting with new onset or changes to preexisting neurologic manifestations. Evaluation of PML includes, but is not limited to, consultation with a neurologist, brain MRI, and lumbar puncture. Discontinue GAZYVA therapy and consider discontinuation or reduction of any concomitant chemotherapy or immunosuppressive therapy in patients who develop PML |
|
| Infusion Reactions |
| • | GAZYVA can cause severe and life-threatening infusion reactions. Sixty percent of patients with previously untreated NHL experienced a reaction on Day 1 of GAZYVA infusion. Infusion reactions can also occur with subsequent infusions. Symptoms may include hypotension, tachycardia, dyspnea, and respiratory symptoms (e.g., bronchospasm, larynx and throat irritation, wheezing, and laryngeal edema). Most frequently reported symptoms include nausea, fatigue, chest discomfort, dyspnea, dizziness, vomiting, diarrhea, rash, hypertension, hypotension, flushing, headache, pyrexia, and chills |
| • | Premedicate patients with acetaminophen, an antihistamine, and a glucocorticoid. Institute medical management for infusion reactions as needed. Closely monitor patients during the entire infusion. Infusion reactions within 24 hours of receiving GAZYVA have occurred |
| • | For patients with any Grade 4 infusion reactions, including but not limited to anaphylaxis, acute life-threatening respiratory symptoms, or other life-threatening infusion reaction: Stop the GAZYVA infusion. Permanently discontinue GAZYVA therapy |
| • | For patients with Grade 1, 2, or 3 infusion reactions: Interrupt GAZYVA for Grade 3 reactions until resolution of symptoms. Interrupt or reduce the rate of the infusion for Grade 1 or 2 reactions and manage symptoms |
| • | For patients with preexisting cardiac or pulmonary conditions, monitor more frequently throughout the infusion and the post-infusion period since they may be at greater risk of experiencing more severe reactions. Hypotension may occur as part of the GAZYVA infusion reaction. Consider withholding antihypertensive treatments for 12 hours prior to and during each GAZYVA infusion, and for the first hour after administration until blood pressure is stable. For patients at increased risk of hypertensive crisis, consider the benefits versus the risks of withholding their antihypertensive medication |
|
| Hypersensitivity Reactions Including Serum Sickness |
| • | Hypersensitivity reactions have been reported in patients treated with GAZYVA. Signs of immediate-onset hypersensitivity included dyspnea, bronchospasm, hypotension, urticaria and tachycardia. Late-onset hypersensitivity diagnosed as serum sickness has also been reported with symptoms that include chest pain, diffuse arthralgia and fever. Hypersensitivity reactions may be difficult to clinically distinguish from infusion related reactions. However, hypersensitivity very rarely occurs with the first infusion and, when observed, often occur after previous exposure. If a hypersensitivity reaction is suspected during or after an infusion, the infusion must be stopped and treatment permanently discontinued. Patients with known hypersensitivity reactions to GAZYVA, including serum sickness, must not be retreated |
|
| Tumor Lysis Syndrome (TLS) |
| • | Tumor lysis syndrome, including fatal cases, has been reported in patients receiving GAZYVA. Patients with high tumor burden, high circulating lymphocyte count (>25 x 109/L) or renal impairment are at greater risk for TLS and should receive appropriate tumor lysis prophylaxis with antihyperuricemics (eg, allopurinol or rasburicase) and hydration prior to the infusion of GAZYVA. During the initial days of GAZYVA treatment, monitor the laboratory parameters of patients considered at risk for TLS. For treatment of TLS, correct electrolyte abnormalities, monitor renal function and fluid balance, and administer supportive care, including dialysis as indicated |
|
| Infections |
| • | Fatal and serious bacterial, fungal, and new or reactivated viral infections can occur during and following GAZYVA therapy. When GAZYVA is administered with chemotherapy followed by GAZYVA monotherapy, Grade 3 to 5 infections have been reported in up to 8% of patients during combination therapy, up to 13% of patients during monotherapy, and up to 8% of patients after treatment. Do not administer GAZYVA to patients with an active infection. Patients with a history of recurring or chronic infections may be at increased risk of infection |
| • | In GALLIUM, more Grade 3 to 5 infections were reported in the recipients of GAZYVA and bendamustine (117/410 patients, 29%), as compared to GAZYVA plus CHOP or CVP (43/281 patients, 15%). More fatal infections were reported in patients treated with GAZYVA and bendamustine (3%), as compared to GAZYVA plus CHOP or CVP (<1%), including during the monotherapy phase and after completion of treatment |
|
| Neutropenia |
| • | Severe and life-threatening neutropenia, including febrile neutropenia, has been reported during treatment with GAZYVA. Monitor patients with Grade 3 to 4 neutropenia frequently with regular laboratory tests until resolution. Anticipate, evaluate, and treat any symptoms or signs of developing infection. Consider administration of granulocyte colony-stimulating factors (GCSF) in patients with Grade 3 or 4 neutropenia |
| • | Neutropenia can also be of late onset (occurring more than 28 days after completion of treatment) and/or prolonged (lasting longer than 28 days) |
| • | Consider dose delays in the case of Grade 3 or 4 neutropenia. Patients with severe and long lasting (>1 week) neutropenia are strongly recommended to receive antimicrobial prophylaxis until resolution of neutropenia to Grade 1 or 2. Consider antiviral and antifungal prophylaxis |
|
| Thrombocytopenia |
| • | Severe and life threatening thrombocytopenia has been reported during treatment with GAZYVA in combination with chemotherapy. Fatal hemorrhagic events have been reported in patients with NHL treated with GAZYVA in combination with chemotherapy, including during Cycle 1. Monitor all patients frequently for thrombocytopenia and hemorrhagic events, especially during the first cycle. In patients with Grade 3 or 4 thrombocytopenia, monitor platelet counts more frequently until resolution and consider subsequent dose delays of GAZYVA and chemotherapy or dose reductions of chemotherapy. Transfusion of blood products (i.e., platelet transfusion) may be necessary. Consider withholding concomitant medications which may increase bleeding risk (platelet inhibitors or anticoagulants), especially during the first cycle |
|
| Immunization |
| • | The safety and efficacy of immunization with live or attenuated viral vaccines during or following GAZYVA therapy have not been studied. Immunization with live virus vaccines is not recommended during treatment and until B-cell recovery |
|
| Pregnancy |
| • | There are no data with GAZYVA use in pregnant women to inform a drug-associated risk. GAZYVA is likely to cause fetal B-cell depletion. GAZYVA should be used during pregnancy and/or breastfeeding only if the potential benefit justifies the potential risk to the fetus and/or infant. Mothers who have been exposed to GAZYVA during pregnancy should discuss the safety and timing of live virus vaccinations for their infants with their child's healthcare providers |
|
| Geriatric Use |
| • | Of the 691 patients in GALLIUM treated with GAZYVA plus chemotherapy as first-line therapy, 33% were 65 and over, while 7% were 75 and over. Of patients 65 and over, 63% experienced serious adverse reactions and 26% experienced adverse reactions leading to treatment withdrawal, while in patients under 65, 43% experienced serious adverse reactions and 13% had an adverse reaction leading to treatment withdrawal. No clinically meaningful differences in efficacy were observed between these patients and younger patients |
|
| Additional Important Safety Information |
| • | A randomized, open-label multicenter trial (GALLIUM) evaluated the safety of GAZYVA as compared to rituximab product in 1,385 patients with previously untreated follicular lymphoma (86%) or marginal zone lymphoma (14%) |
| • | Serious adverse reactions occurred in 50% of patients on the GAZYVA arm and 43% of patients on the rituximab product arm. Fatal adverse reactions were reported during treatment in 3% in the GAZYVA arm and 2% in the rituximab product arm, most often from infections in the GAZYVA arm. During treatment and follow-up combined, fatal adverse reactions were reported in 5% of the GAZYVA arm and 4% of the rituximab product arm, with infections and second malignancies being leading causes. In the GAZYVA arm, fatal infections occurred in 2% of patients compared to <1% in the rituximab product arm |
| • | Neutropenia, infusion related reactions, febrile neutropenia and thrombocytopenia were the most common Grade 3 to 5 adverse reactions (incidence ≥5%) observed more frequently in the GAZYVA arm |
| • | Throughout treatment and follow-up, the most common adverse reactions (incidence ≥20%) observed at least 2% more in the GAZYVA arm were infusion related reactions (72%), neutropenia (53%), upper respiratory tract infection (50%), cough (35%), constipation (32%) and diarrhea (30%) |
| • | During the monotherapy period, the common adverse reactions (incidence ≥10%) observed at least 2% more with GAZYVA were upper respiratory infection (40%), cough (23%), musculoskeletal pain (20%), neutropenia (19%) and herpesvirus infection (13%) |
|
|
|
|
|
|
| INDICATION |
| GAZYVA, in combination with chemotherapy followed by GAZYVA monotherapy in patients achieving at least a partial remission, is indicated for the treatment of adult patients with previously untreated stage II bulky, III or IV follicular lymphoma (FL). |
| IMPORTANT SAFETY INFORMATION |
| BOXED WARNINGS: HEPATITIS B VIRUS REACTIVATION AND PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY |
| • | Hepatitis B Virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients receiving CD20-directed cytolytic antibodies, including GAZYVA. Screen all patients for HBV infection before treatment initiation. Monitor HBV positive patients during and after treatment with GAZYVA. Discontinue GAZYVA and concomitant medications in the event of HBV reactivation |
| • | Progressive Multifocal Leukoencephalopathy (PML) including fatal PML, can occur in patients receiving GAZYVA |
|
| Contraindications |
| • | GAZYVA is contraindicated in patients with known hypersensitivity reactions (e.g. anaphylaxis) to obinutuzumab or to any of the excipients, or serum sickness with prior obinutuzumab use |
|
| Warnings and Precautions |
| Hepatitis B Virus (HBV) Reactivation |
| • | Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients treated with anti-CD20 antibodies including GAZYVA. HBV reactivation has been reported in patients who are hepatitis B surface antigen (HBsAg) positive and in patients who are HBsAg negative but are hepatitis B core antibody (anti-HBc) positive. Reactivation has also occurred in patients who appear to have resolved hepatitis B infection (ie, HBsAg negative, anti-HBc positive, and hepatitis B surface antibody [anti-HBs] positive) |
| • | HBV reactivation is defined as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA level, or detection of HBsAg in a person who was previously HBsAg negative and anti-HBc positive. Reactivation of HBV replication is often followed by hepatitis, ie, increase in transaminase levels and, in severe cases, increase in bilirubin levels, liver failure, and death |
| • | Screen all patients for HBV infection by measuring HBsAg and anti-HBc before initiating treatment with GAZYVA. For patients who show evidence of hepatitis B infection (HBsAg positive [regardless of antibody status] or HBsAg negative but anti-HBc positive), consult physicians with expertise in managing hepatitis B regarding monitoring and consideration for HBV antiviral therapy |
| • | Monitor patients with evidence of current or prior HBV infection for clinical and laboratory signs of hepatitis or HBV reactivation during and for several months following treatment with GAZYVA |
| • | In patients who develop reactivation of HBV while receiving GAZYVA, immediately discontinue GAZYVA and any concomitant chemotherapy and institute appropriate treatment. Resumption of GAZYVA in patients whose HBV reactivation resolves should be discussed with physicians with expertise in managing hepatitis B. Insufficient data exist regarding the safety of resuming GAZYVA in patients who develop HBV reactivation |
|
|
|




Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου