Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report
Category: Trauma
Article Type: Case Report
Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito
Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
Correspondence Address:
Ryo Hiruta
Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
DOI:10.25259/SNI-235-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
How to cite this article: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79
How to cite this URL: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79. Available from: http://surgicalneurologyint.com/surgicalint-articles/acute-paradoxical-brain-herniation-after-decompressive-craniectomy-for-severe-traumatic-brain-injury-a-case-report/
Category: Trauma
Article Type: Case Report
Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito
Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
Correspondence Address:
Ryo Hiruta
Department of Neurosurgery, Fukushima Medical University, 1 Hikarigaoka, Fukushima, Japan
DOI:10.25259/SNI-235-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
How to cite this article: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79
How to cite this URL: Ryo Hiruta, Shinya Jinguji, Taku Sato, Yuta Murakami, Mudathir Bakhit, Yosuke Kuromi, Keiko Oda, Masazumi Fujii, Jun Sakuma, Kiyoshi Saito. Acute paradoxical brain herniation after decompressive craniectomy for severe traumatic brain injury: A case report. 10-May-2019;10:79. Available from: http://surgicalneurologyint.com/surgicalint-articles/acute-paradoxical-brain-herniation-after-decompressive-craniectomy-for-severe-traumatic-brain-injury-a-case-report/
Background:Sinking skin flap syndrome or paradoxical brain herniation is an uncommon neurosurgical complication, which usually occurs in the chronic phase after decompressive craniectomy. We report a unique case presenting with these complications immediately after decompressive craniectomy for severe traumatic brain injury.
Case Description:A 65-year-old man had a right acute subdural hematoma (SDH), contusion of the right temporal lobe, and diffuse traumatic subarachnoid hemorrhage with midline shift to the left side. He underwent an emergency evacuation of the right SDH with a right decompressive frontotemporal craniectomy. Immediately after the operation, his neurological and computed tomography (CT) findings had improved. However, within 1 h after the surgery, his neurological signs deteriorated. An additional follow-up CT showed a marked midline shift to the left, i.e., paradoxical brain herniation, and his skin flap overlying the decompressive site was markedly sunken. We immediately performed an urgent cranioplasty with the right temporal lobectomy. He responded well to the procedure. We suspected that a cerebrospinal fluid leak had caused this phenomenon.
Conclusion:Decompressive craniectomy for severe traumatic brain injury can lead to sinking skin flap syndrome and/or paradoxical brain herniation even in the acute phase. We believe that immediate cranioplasty allows the reversal of such neurosurgical complications.
Keywords: Paradoxical brain herniation, Traumatic brain injury, Decompressive craniectomy, Intracranial hypotension, Neurosurgery
INTRODUCTION
Sinking skin flap syndrome, also known as “syndrome of the trephined,” is an uncommon complication after decompressive craniectomy. This condition involves sinking of the scalp on the decompressed side deep beyond the edges of the bone defect.[ 15 ] Although it is very rare, sinking skin flap syndrome may lead to paradoxical brain herniation, which is defined as brain herniation in the contralateral side to the decompressed area. This, in turn, leads to severe neurological deterioration such as comatose state, anisocoria, and decerebrate rigidity.[ 1 , 6 ] Lower intracranial pressure compared to extracranial pressure causes these phenomena.[ 1 , 3 ] In the acute traumatic phase, many patients develop brain swelling at the decompressed hemisphere due to the traumatic brain edema.[ 4 ] Hence, these complications often occur at the chronic traumatic phase, i.e., within several weeks to months from an injury when the intracranial pressure is declining.[ 1 - 3 , 11 ] We herein report a case of paradoxical brain herniation within 1 h after a decompressive craniectomy for severe traumatic brain injury.
CASE REPORT
A 65-year-old man was found unconscious with bleeding from a left side scalp wound at the bottom of the stairs in his house where he seemed to have fallen down. On arrival at the hospital, his Glasgow Coma Scale (GCS) score was 5 (E1V1M3) without anisocoria. He had a laceration in his left frontotemporal scalp but presented with no other injuries on his trunk or extremities. There were no apparent findings of cerebrospinal fluid (CSF) leakage. However, within 20 min of arrival at the hospital, the diameter of his right pupil changed from 3 mm to 6 mm, although that of the left pupil remained 3 mm. He was immediately intubated. A plain brain computed tomography (CT) showed a right acute subdural hematoma (SDH), contusion of the right temporal lobe, traumatic subarachnoid hemorrhage, and midline shift to the left side [ Figure 1a ]. The CT also showed a linear fracture of the left temporoparietal bone and a small fracture at the frontal skull base. There was no evidence of other bone fractures, such as in the spinal bone, and any other organ injury on CT. He underwent an emergency evacuation of the right SDH. The surgeon had the impression that the brain could swell as a result of the severe injury. Therefore, it was decided to do a right frontotemporal decompressive craniectomy, and the dura was closed using a Gore-Tex membrane graft. The size of his skull defect was approximately 10 cm × 11 cm2.
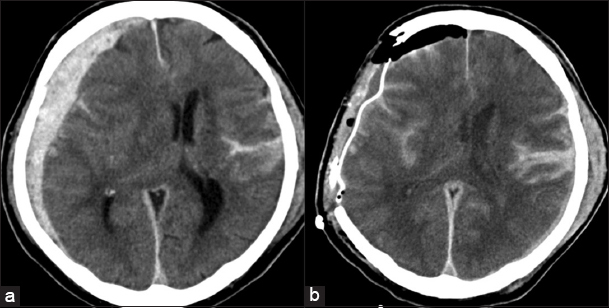
Figure 1
(a) Axial plain of brain computed tomography obtained before the initial surgery showing a right acute subdural hematoma, brain contusion, traumatic subarachnoid hemorrhage, and midline shift to the left side measuring approximately 1.5 cm in thickness. (b) Axial plain brain computed tomography obtained right after the initial surgery showing decompressive right frontotemporal craniectomy and improvement of the midline shift.
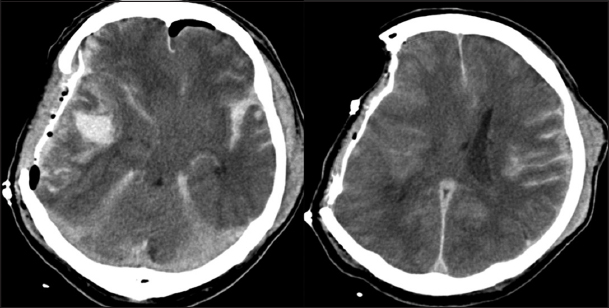
After the operation, his anisocoria improved: the right pupil was 3 mm and the left pupil was 1.5 mm, and plain brain CT showed a regression of the mass effect and midline shift [ Figure 1b ]. However, within 1 h after the surgery, the anisocoria worsened: the right pupil was 6 mm and the left pupil was 2 mm. An additional CT scan showed a marked midline shift from the right to the left side with brain herniation, i.e., direction opposite to the craniectomy side, compared to the previous CT [ Figure 2 ]. The scan also showed that the skin flap overlying the decompressive craniectomy site was markedly sunken [ Figure 3 ]. Although the optimal course of action was unclear, we suspected in that situation the atmospheric pressure did exceed the intracranial pressure around the decompressive craniectomy site, resulting in “sinking skin flap syndrome,” which usually occurs in the chronic phase after the decompressive craniectomy. We immediately performed lobectomy of contusion of the right temporal lobe as a precaution for any further brain swelling might occur. Next, cranioplasty was performed using the autologous bone. After the second operation, the patient’s pupils were constricted (2 mm in the right pupil and 1.5 mm in the left pupil). A follow-up CT showed significant improvement of the midline shift [Figure 4a ]. An intracranial pressure monitoring sensor was placed into the right frontal lobe during the second operation. The primary reading was 4 cm H2O immediately after the second operation and 10–15 cm H2O on the following days. We suspected that a CSF leak had caused his intracranial hypotension. To confirm our hypothesis, we aimed at detecting the CSF leakage site using CT myelography 3 days later. Unfortunately, we were unable to conduct the investigation because the lumbar puncture resulted in a dry tap.
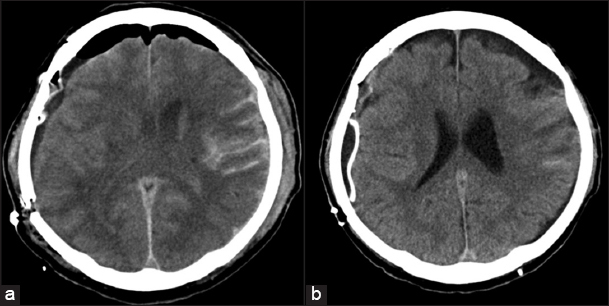
Figure 4
(a) Axial plain brain computed tomography obtained right after the second surgery showing improvement and resolution of the midline shift, which was recognized after the initial surgery. (b) Axial plain brain computed tomography obtained 14 days after the second surgery showing no additional abnormal findings compared to that obtained after the second surgery.
A follow-up CT scan 2 weeks later showed complete resolution of the midline shift [ Figure 4b ]. We did not perform further investigation to confirm the CSF pressure state because there was no evidence suggesting low CSF pressure, such as that in bilateral chronic SDH or tonsillar herniation. Furthermore, his general condition was unstable at the time. One month after the trauma and the two operations, he was transferred to a rehabilitation hospital. His GCS score was 9 (E4VTM4) and breathing through a tracheostomy tube. He is now bedridden and requires a feeding tube.
DISCUSSION
In the present case, we performed decompressive craniectomy to treat a severe head injury. However, the patient experienced paradoxical brain herniation in the immediate postoperative period. We suspected that his serious condition was similar to sinking skin flap syndrome and, therefore, performed an immediate cranioplasty. The patient responded to the treatment well and showed no further deterioration.
In many cases of severe brain injury that requires decompressive craniectomy, brain swelling may occur toward the decompressed area due to the elevating intracranial pressure of the injured brain.[ 4 ] However, some patients who underwent decompressive craniectomy have been reported to have experienced a paradoxical brain herniation after CSF drainage, including lumbar puncture, extraventricular drainage, or ventriculoperitoneal shunt.[ 5 , 6 , 11 , 14 ] These phenomena were reported as delayed complications. However, it is reported that the patient did develop a paradoxical brain herniation on the following day after decompressive craniectomy for head trauma with CSF rhinorrhea.[ 8 ] In our patient, the cause of head trauma suspected to be due to a fall down the stairs. Hence, there was a possibility that CSF leakage occurred from the cervical or lumbar region of the spine caused by dural laceration. It has been reported that intracranial hypotension following CSF leakage is associated with head injury.[ 7 , 13 ] Therefore, in the current case, we performed a lumbar puncture for CT myelography to detect the points of CSF leakage using a radioscopic examination apparatus, but it was a dry tap. Although we could not perform CT myelography, we suspected that a dry tap could support the idea of a CSF leak.
The first step of treatment for sinking skin flap syndrome or paradoxical brain herniation is similar to that of treatment for intracranial hypotension, i.e., correction of the intracranial pressure, which is exceeded by extracranial pressure.[ 1 , 5 ] In this kind of situation, we would place the patient in the Trendelenburg position and perform hydration and clamping of the CSF drainage if available. If the point of CSF leak was detected, a blood patch would be effective.[ 9 ]
It is generally agreed on that cranioplasty is the definitive treatment for sinking skin flap syndrome and paradoxical brain herniation.[ 1 , 6 , 9 ] The efficacy of cranioplasty was also demonstrated in our case. The sinking skin flap in the craniectomy site and the deterioration of the neurological findings occurred within 1 h. We speculated that the intracranial pressure in our case exceeded by the atmospheric pressure on the basis of low intracranial pressure due to CSF leakage. We considered that the cranioplasty could control this condition. However, we supposed that there would be a risk of an increase in his intracranial pressure after cranioplasty. Therefore, during the second operation, we performed resection of the bruised right temporal lobe in addition to the cranioplasty. In the second operation, we could not only correct his low intracranial pressure but also prevented elevation of his intracranial pressure due to the severe head injury.
Although craniotomy and decompressive craniectomy are both used in acute SDH, yet it is not clear which one is the most appropriate. The decision to perform a decompressive craniectomy is usually based on the personal judgment of the neurosurgeons.[ 12 ] Craniectomy is often performed in patients who have the risk of brain swelling and increasing of the ICP.[ 10 ] During the surgery, even in the absence of any signs of focal brain swelling, it remains unclear if the bone flap should be removed as a precaution. Based on our experience with the current case, we suggest if there is no focal brain swelling, the bone flap could be placed back.
CONCLUSION
A decompressive craniectomy for a severe traumatic brain injury may induce “acute paradoxical brain herniation,” and may lead to sudden neurological deterioration. Although such situations are infrequent, we suggest that immediate cranioplasty is required to improve such complications as well as to prevent further implications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understanding that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akins PT, Guppy KH. Sinking skin flaps, paradoxical herniation, and external brain tamponade:A review of decompressive craniectomy management. Neurocrit Care. 2008. 9: 269-76
2. Annan M, De Toffol B, Hommet C, Mondon K. Sinking skin flap syndrome (or Syndrome of the trephined):A review. Br J Neurosurg. 2015. 29: 314-8
3. Ashayeri K, Jackon EM, Huang J, Brem H, Gordon CR. Syndrome of the trephined:A systematic review. Neurosurgery. 2016. 79: 525-34
4. Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM. Decompressive craniectomy:A meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012. 117: 589-96
5. Creutzfeldt CJ, Vilela MD, Longstreth WT. Paradoxical herniation after decompressive craniectomy provoked by lumbar puncture or ventriculoperitoneal shunting. J Neurosurg. 2015. 123: 1170-5
6. Fields JD, Lansberg MG, Skirboll SL, Kurien PA, Wijman CA. “Paradoxical” transtentorial herniation due to CSF drainage in the presence of a hemicraniectomy. Neurology. 2006. 67: 1513-4
7. Hasheminia D, Motamedi MR, Hashemzehi H, Nazeri R, Movahedian B. A 7-year study of 1,278 patients with maxillofacial trauma and cerebrospinal fluid leak. J Maxillofac Oral Surg. 2015. 14: 258-62
8. Ji H, Chen W, Yang X, Guo J, Wu J, Huang M. Paradoxical herniation after unilateral decompressive craniectomy:A retrospective analysis of clinical characteristics and effectiveness of therapeutic measures. Turk Neurosurg. 2017. 27: 192-200
9. Muehlschlegel S, Voetsch B, Sorond FA. Emergent epidural blood patch:Lifesaving treatment of paradoxical herniation. Arch Neurol. 2009. 66: 670-1
10. Phan K, Moore JM, Griessenauer C, Dmytriw AA, Scherman DB, Sheik-Ali S. Craniotomy versus decompressive craniectomy for acute subdural hematoma:Systematic review and meta-analysis. World Neurosurg. 2017. 101: 677-85
11. Ramos-Zuniga R, Mares-Pais R, Gutierrez-Avila O, Saldana-Koppel DA. Paradoxical herniation in the postcraniectomy syndrome:Report and literature update. J Neurol Surg Rep. 2016. 77: e035-8
12. Rush B, Rousseau J, Sekhon MS, Griesdale DE. Craniotomy versus craniectomy for acute traumatic subdural hematoma in the United States:A national retrospective cohort analysis. World Neurosurg. 2016. 88: 25-31
13. Sarrafzadeh AS, Hopf SA, Gautschi OP, Narata AP, Schaller K. Intracranial hypotension after trauma. Springerplus. 2014. 3: 153-
14. Watanabe J, Maruya J, Nishimaki K. Sinking skin flap syndrome after unilateral cranioplasty and ventriculoperitoneal shunt in a patient with bilateral decompressive craniectomy. Interdiscip Neurosurg. 2016. 5: 6-8
15. Yamaura A, Sato M, Meguro K, Nakamura T, Uemura K. Cranioplasty following decompressive craniectomy analysis of 300 cases. No Shinkei Geka. 1977. 5: 345-53

Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου